Oral Surgery
Below are some frequently asked questions about oral surgery. We have a separate dedicated page regarding the Removal of Wisdom Teeth. Please contact us if you have any specific queries, or book an appointment to see us for a consultation.
Why see a specialist?
Specialists are dentists that have significant experience and training in their chosen field and are recognised for this by the General Dental Council. Your general dentist will be very capable of carrying out the majority of your treatment however, there will be occasions where due to the complexity of treatment they would prefer to refer you to a specialist.
Even for routine treatments, we are usually able to carry out the same treatment with more speed and efficiency due to our experience.
Can I get oral surgery treatment on the NHS?
Yes, however, we do not have the ability to receive personal NHS referrals directly. We have been working for the NHS at Guy’s Hospital for over 10 years, so we fully appreciate this service, but there are benefits to choosing a private referral to see us directly.
Some reasons you may choose a private referral to see us:
- You know who you will be seeing and can rest assured that you will get a personal level of care. You cannot choose who to see on the NHS and are not guaranteed to see a specialist for treatment. Also, if you require several appointments, it is not guaranteed that you would see the same person twice in the hospital, whereas with us, you can count on having the same familiar team always looking after you.
- NHS departments and reception rooms are often very busy. In contrast, in our practice you will be in a familiar and comfortable surrounding.
- And the obvious one – waiting times. With the amount of burden on the NHS, waiting times can be in the region of several months for non-urgent treatment from the time your dentist refers you. If you require further investigations and appointments, there can again be a long wait between these. With private referrals, there is virtually no waiting and investigations are fast-tracked and streamlined.
What is oral surgery?
The specialty of Oral Surgery deals with the diagnosis and management of pathology of the mouth and jaws that requires surgical intervention.
Common oral surgery procedures include:
- routine or complex extractions
- wisdom teeth extractions, including impacted teeth
- extractions at high risk of nerve damage
- coronectomy
- expose and bond of ectopic teeth
- management of medically compromised patients including bisphosphonates
- biopsy of soft tissues
- biopsy of benign lumps and bumps such as mucoceles
- biopsy of dento-alveolar cysts
- frenectomy
- tongue-tie release
Is oral surgery treatment painful?
Not really! Treatment is carried out under local anaesthetic, so you will be fully numb, and other than some movement and pressure there will not be any pain. Of course as with any minor oral surgery, there is some discomfort expected following the surgery, but this is manageable with over the counter painkillers and settles down rather quickly. Some procedures can result in more soreness and swelling than others and we will discuss your specific case with you in detail.
Can I be put to sleep for oral surgery?
Being fully asleep is known as a general anaesthetic. This is something that is not available in a dental practice and is only carried out in hospitals.
If you are anxious and like the idea of being asleep, we can usually carry out your treatment under intravenous sedation instead. This is a form of ‘conscious sedation’ where you are given a drug through a drip into your vein, and whilst you will not be asleep, most people are so relaxed that they often feel like they were asleep and do not often recall anything about the treatment. It is a very safe and commonly carried out procedure, even for routine treatments if someone is anxious, and we will be happy to discuss your suitability for sedation.
Even if you are not a nervous patient, we may sometimes advise that your treatment is actually best carried out under sedation. This is usually due to the complexity of treatment. Even though the treatment is not painful, the reality is that some surgical treatments may not be particularly comfortable, and we feel that making sure our patients are as comfortable as possible is of the highest priority.
Finally, some treatments may indeed be best carried out under a general anaesthetic, but this is strictly judged on a clinical need and not a personal preference to be asleep. This is due to the additional health risks involved with a general anaesthetic. We will be happy to discuss your options for NHS or private hospital referral if deemed necessary.
What is a dental extraction?
Extraction means the complete removal of a tooth and its roots. This is usually carried out when the tooth is no longer salvagable or if it poses a risk to the surrounding area if it remains in the mouth.
Extractions are usually referred to as a ‘routine’ or ‘surgical’ extraction, where the latter involves the use of a small drill, similar to having a filling, to remove a tooth.
What are wisdom teeth and why do they cause problems?
Wisdom teeth are the last teeth to grow in the mouth, usually from the late teens onwards. They are the third set of molar teeth in the mouth, and are also referred to as ‘3rd molars’. They are just normal teeth otherwise.
The reason that they are known to cause problems is to do with the limited space that they have to grow into. It is very common to not have enough space for a wisdom tooth at the back of the mouth, causing it to become stuck – either against the gums, bone or the adjacent tooth. This is not always a problem but it is common to experience food trapping around the wisdom tooth, which can cause pain and swelling of the gums – known as pericoronitis. Food trapping can also cause decay in the adjacent tooth. If these problems are significant, then we usually consider removing the wisdom teeth.
Do all wisdom teeth have to be removed?
No.
Generally speaking, we only remove wisdom teeth that have something wrong with them, cause recurrent problems, or pose a significant risk of causing further damage if left alone. Some of these problems may not be obvious to you, which is why regular check-ups is essential for your dentist to spot any potential problems early.
Some wisdom teeth do not grow into the mouth at all and remain buried underneath the gum. If they are fully buried, these teeth generally do not cause any problems and can be left and monitored. But some may develop pathological problems around them, such as balloon like swellings known as cysts. These generally should not be left alone and require removal.
Do wisdom teeth make the front teeth crooked?
No.
This is a common myth, which is understandable as the front teeth becoming crooked (we call this ‘anterior crowding’) usually coincides with the time that wisdom teeth tend to start growing. But wisdom teeth simply do not have the potential to push all of your teeth to the extent to cause anterior crowding, and there is evidence to show this.
There are several reasons for anterior crowding, usually related to age and skeletal/dental growth rates or if you had braces as a child without long-term retainers.
My dentist has said my tooth is too close to a nerve for them to extract?
This is likely a nerve we call the inferior dental nerve, or the IDN for short. This is a feeling nerve, and provides feeling to the skin and gums on the same side as the nerve, up to the lower lip and chin areas. When a dentist numbs a tooth on the lower jaw with local anaesthetic, this is the nerve that becomes numb.
Sometimes a tooth is positioned in a very close proximity to this nerve, and the removal of the tooth can pose a risk of damaging the nerve in the process. This can cause temporary, or rarely permanent, altered sensation to the lower lip, chin, tongue, gums and teeth areas. This altered sensation is usually a tingling or numbness but it can also be a sensation such as burning, stabbing or shooting pains. The risk of this occuring varies significantly between different teeth and is assessed on a case by case basis.
As it happens, due to the anatomy of the jaws, it is usually the lower wisdom teeth that end up being close to this nerve, but any of the other lower back teeth can also be close depending on their position and size.
Your dentist has probably judged the proximity of this nerve based on a conventional 2D X-ray. We may advise that based on our experience, the tooth is in fact not close enough to be a problem. Nevertheless, the 2D X-ray does not provide a full picture and we may advise a 3D Cone Beam CT (CBCT) scan to find out exactly where the nerve is positioned in relation to the tooth. This may either show that the nerve was in fact not as close as it looked, and the risk of any nerve damage is low, or it may confirm that the nerve is indeed closely related to the tooth. Depending on the individual situation, if we have decided that leaving the tooth and monitoring is not an option, we may then recommend a coronectomy procedure.
What is a coronectomy?
Coronectomy literally means ‘removal of crown’. This is a small surgical procedure where the top of the tooth, or the crown, is removed with a small drill. The remainder of the tooth roots are smoothened below the gum and bone, and the gums are stitched to close the tooth gap.
This removes the problem area of the tooth, which is usually the crown, but avoids disturbing the roots of the tooth that may be close to the nerve explained above.
As far as the patient is concerned, the procedure itself is no different to having the whole tooth removed. The roots of the tooth generally remain buried and do not cause any further problems, but in a small minority of cases, these roots do cause discomfort and/or infections. This may mean that the roots may have to be surgically removed at a later date however, usually the roots move up and away from the nerve following a coronectomy. So if they require removal later, the risk to the nerve is usually lower.
Although this is not a complex procedure per se, it is rather technique sensitive and needs to be carried out in a specific way. Some dentists who are not particularly familiar with or do not carry out many coronectomies may not advocate this as a good treatment option. However, there is ample scientific evidence in support of the efficacy and safety of coronectomies, some of which we have published ourselves, and with a good understanding of the procedure and in the right hands, it is an effective option for high risk cases.
My dentist has said that my tooth is too close to my sinus for them to extract?
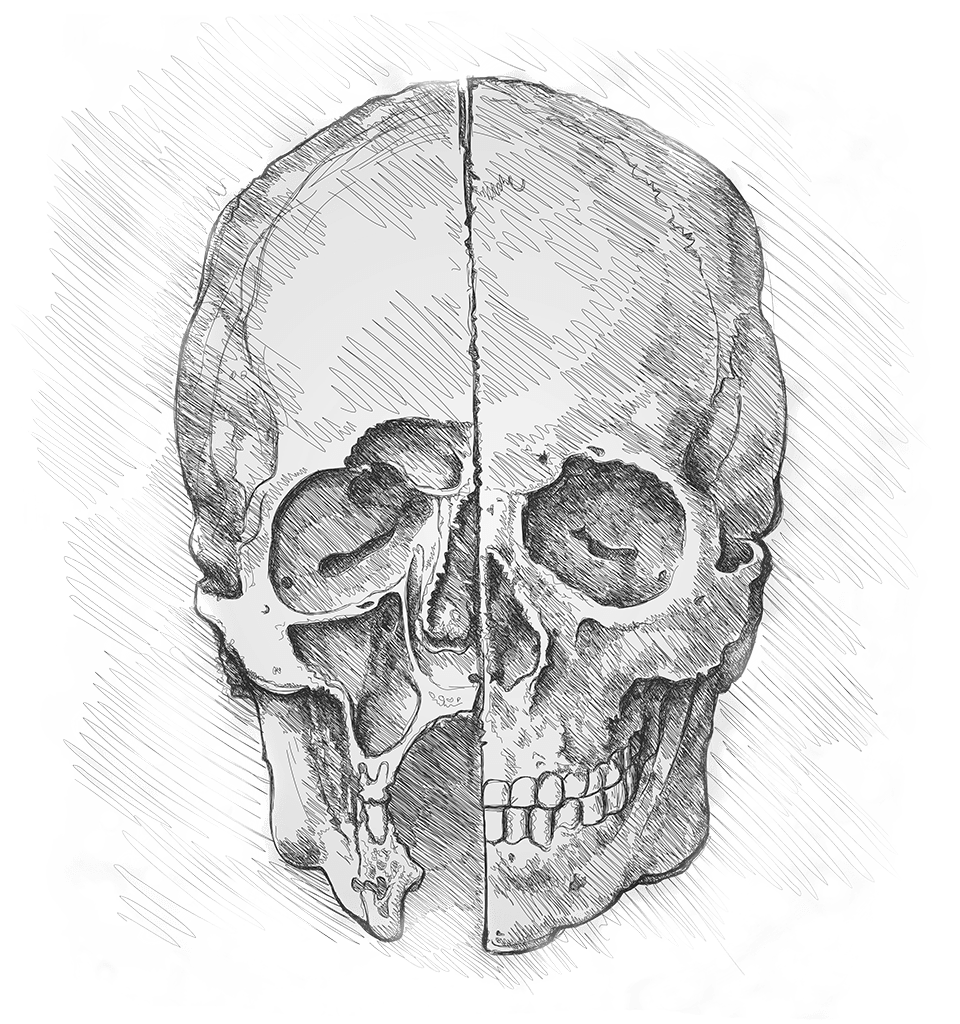
This is called the maxillary sinus, and is an air space above your teeth inside the skull. You can actually see this space in the image at the top of this page!
Sometimes the roots of the upper back teeth can be close to this sinus, and the removal of the tooth may cause a hole between the gums and the sinus, called an oro-antral communication (or OAC). This is actually a lot less common than a lot of dentists think, and many of the teeth that your dentist may be concerned about are actually at a very low risk of having this problem.
Of course some teeth will have a high risk of developing an OAC. If this happens and the hole is small, sometimes nothing needs to be done other than close monitoring and the hole closes spontaneously as the gums heal. If the hole is big, it is unlikely to close by itself and will require a small surgical procedure to close the hole. This can either be carried out at the same time as the extraction, or it can be at a later date.
Some of the symptoms of an OAC once the gums have healed are a bad taste or discharge from the site of the tooth extraction or a discharge from the nostril on the same side as the extraction when drinking fluids.
Where can I find out more?
We have some more detail about wisdom teeth in our dedicated page – Removal of Wisdom Teeth
The British Association of Oral Surgeons provides useful patient information leaflets: BAOS Patient Information Leaflets
Of course we would love to hear from you personally if you have any queries, or if you would like to see us for a consultation – Contact